Planovar Period Reset in Japan: Schedule, Side Effects, and Safety
“I was prescribed Planovar, but when will my period come? Are the side effects manageable? Will it interfere with my wedding or travel plans?”
Even if your gynecologist recommended a period reset with Planovar, you may still feel anxious about the exact process and its effects on your body. For those with important upcoming events such as weddings or travel, adjusting the menstrual cycle is not just health management—it can directly affect life’s biggest milestones.
This article answers common concerns such as:
- How many days after the last dose of Planovar will your period start?
- How can you minimize side effects such as nausea and headaches?
- When will ovulation occur after a reset—and how should you plan for conception?
We will explain the mechanism of the period reset using Planovar in plain English and based on medical evidence so that you can proceed with confidence. At Personal Care Clinic, counseling is available to help you adjust your cycle according to your lifestyle and future plans, so do not hesitate to reach out with personal concerns.

At Personal Care Clinic, the morning-after pill can be delivered in as little as 37 minutes.
The prescription process takes just 5 minutes, and if you apply before 10:30 AM, same-day pickup is available (depending on your area).
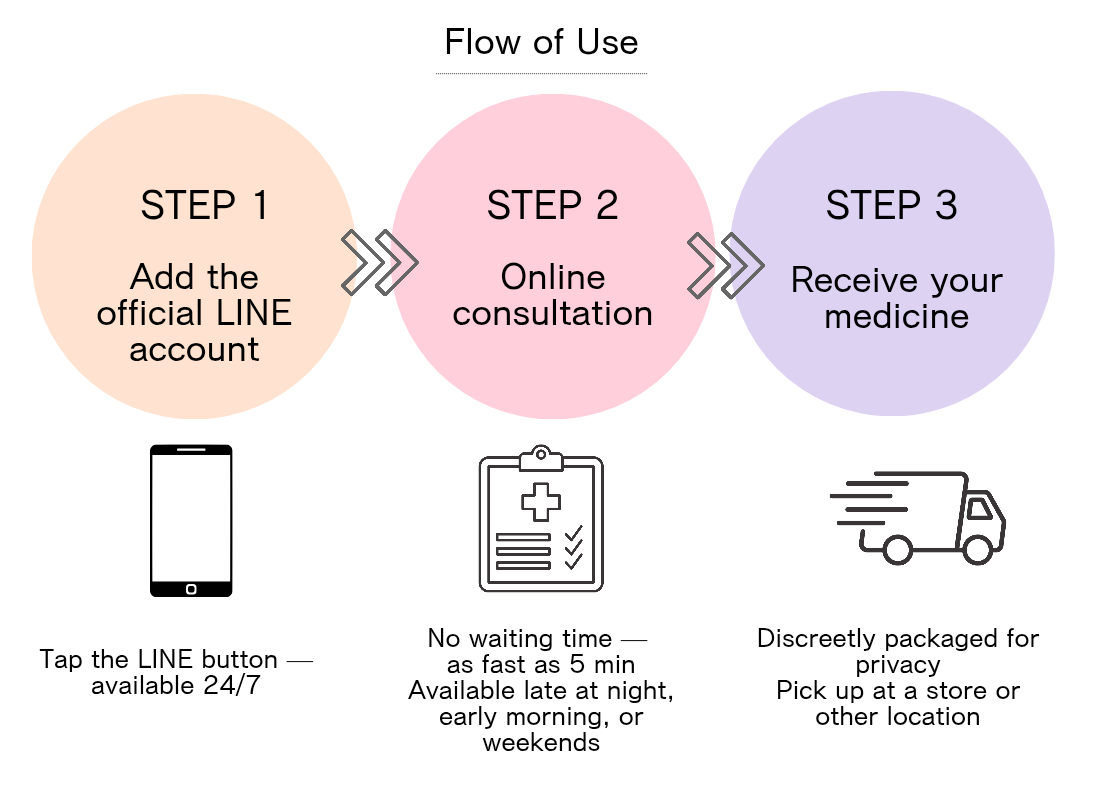
If you want to receive the morning-after pill discreetly, tap the button below to apply now.
What Is a Planovar Period Reset? Basics and Mechanism

A period reset with Planovar is a treatment that restores a regular menstrual cycle by balancing hormones. To use it effectively, it is important to first understand the basic mechanism.
- The ingredients and hormonal effects of Planovar
- Expected outcomes and goals of a period reset
- How it differs from other menstrual regulation drugs
The Ingredients and Hormonal Effects of Planovar
“What exactly is in this medicine? How does it act on the body?” Many patients wonder about this. Planovar contains norgestrel, a type of progestin (yellow body hormone), and ethinylestradiol, a synthetic estrogen (follicle hormone).
These two hormones work together: they thicken the endometrium (uterine lining) to a certain level, and once the medication is stopped, the sudden drop in hormone levels triggers endometrial shedding (menstruation). In a natural cycle, this process is driven by the body’s own hormones, but when hormonal balance is disrupted, Planovar can artificially reproduce this cycle to “reset” menstruation.
Expected Outcomes and Purpose of a Period Reset
“What are the actual benefits of a period reset? In which cases is it used?” A Planovar period reset can help normalize irregular menstrual cycles and improve amenorrhea (no menstruation for long periods). It is particularly useful in conditions related to hormonal imbalance such as ovulatory disorders, endometriosis, or polycystic ovary syndrome (PCOS).
For those with important events like weddings or travel, the ability to predict and adjust menstruation is a huge advantage. However, remember that this is only a temporary solution to manage symptoms—it is not a fundamental treatment. For long-term management, consultation with a gynecologist is essential.
How Planovar Differs from Other Menstrual Regulation Medicines
“How is it different from low-dose birth control pills or herbal remedies? Which is right for me?” The main differences are purpose and duration. Planovar is typically used for a short course (about 7–10 days) to reset menstruation and is valued for its quick effect.
By contrast, low-dose birth control pills also provide contraception and are taken continuously to stabilize cycles. Kampo (traditional Japanese herbal medicine) aims to improve constitution and may take longer to show results, but tends to cause fewer side effects. Planovar is best suited when you need to adjust your cycle for a scheduled event, while low-dose pills may be better for reducing menstrual pain and long-term regulation. The best choice depends on your body, goals, and lifestyle, so consult with your physician to decide.
Specific Schedule for a Planovar Period Reset

When using Planovar for a period reset, both the timing and duration of intake determine its effectiveness. Let’s look at how to create the best schedule for your needs and avoid mistakes.
- Average number of days from last tablet to menstruation
- Different intake patterns depending on whether you want to bring your period forward or delay it
- Timeline adjustment strategies before travel or weddings
Days From Last Dose to Menstruation
“After finishing Planovar, when will my period actually come? I need to plan.” This is one of the most common concerns. In general, withdrawal bleeding (menstruation) occurs about 2–4 days after the last dose. For example, if you complete 10 days of medication, bleeding often starts around day 11–13.
However, this is just an average guideline—individual variation is common. Some first-time users may bleed the day after the last pill, while for others it may take up to 5 days. Your reaction depends on factors such as constitution, age, and hormone status. The first cycle especially should be planned with extra flexibility. Also note that bleeding is often lighter than a natural period and may last only about 3–5 days.
Patterns for Bringing Period Forward or Delaying It
“My trip is coming up—can I make my period earlier or later?” This is a frequent scenario. To bring menstruation forward, start Planovar in the luteal phase (second half of the cycle). For a typical 28-day cycle, starting around day 14 or later can trigger earlier withdrawal bleeding. For example, beginning on day 25 may cause your period to start soon after stopping the pills.
To delay menstruation, begin taking Planovar about 5–7 days before the expected period and continue until your important event is over. For example, if your period is due on day 25, starting on day 20 and continuing past the event can successfully delay bleeding. Always follow medical advice, especially with longer courses, since side effects can increase with extended use.
Timeline Adjustment Strategies for Weddings or Travel
“It would be a nightmare if my wedding day fell on my period!” Many share this concern. The key to successful adjustment before an important event is planning with plenty of margin. Ideally, consult your gynecologist 3–4 weeks before the event. Share your exact date so they can help you set a plan. For a wedding, for example, it is safest to complete menstruation at least two weeks before the ceremony.
Here’s a practical approach: ① Count backward from your event date to set the ideal menstruation end date. ② Set the expected start date 5–7 days before that. ③ With your doctor, create a Planovar schedule that matches this target. If it is your first time, consider a “trial run” to learn how your body responds (days until bleeding, severity of side effects). Always allow about a one-week margin for possible variation. This will help you stay worry-free for your big day.
At Personal Care Clinic, we provide tailored scheduling support to help you manage menstruation with confidence for important life events.
Side Effects of a Planovar Period Reset and How to Manage Them

Side effects from Planovar vary from person to person, but knowing them in advance can ease anxiety and help you cope appropriately. Here we explain actual frequency rates and practical countermeasures so you can prepare with confidence.
- Common side effects and how often they occur
- Over-the-counter remedies and self-care for nausea and headaches
- Warning signs during or after treatment that require medical attention
Common Side Effects and Frequency
“Will I definitely experience side effects? How common are they?” About 20–30% of users report some side effects, but most are mild and temporary. The most frequent are nausea (15–20%), headache (10–15%), and breast tenderness (about 10%). Others include mood changes (about 8%), swelling (5–10%), and irregular bleeding (around 5%).
These usually appear within 2–3 days after starting the pills and often gradually ease as the body adapts. Many users experience no side effects at all, saying, “It wasn’t as difficult as I feared.” Because reactions differ widely, it is important to monitor your own body and consult your doctor if symptoms become difficult to manage.
Learn more about Planovar side effects here ≫
Relieving Nausea and Headaches: OTC Medicine and Self-Care
“I have work but the nausea is tough—what can I do?” Practical strategies include taking Planovar at bedtime, when lying down reduces strain on the stomach. Taking the pill after meals, drinking ginger tea, inhaling menthol, or applying a cold towel to the neck may also help.
For headaches, you may consider over-the-counter pain relievers such as acetaminophen—always confirm with your gynecologist first. Staying well-hydrated, limiting caffeine, taking a warm shower, and stretching the neck and shoulders can also help. For mood swings, practice stress relief techniques such as deep breathing, light exercise, or listening to music. If symptoms become severe, consult your doctor for tailored strategies for next time.
Warning Symptoms That Require Medical Attention
“What signs mean I should go to the hospital right away?” This is critical for safe use. Seek medical care immediately if you experience: ① severe abdominal or calf pain/swelling, ② vision changes or strong headache, ③ chest pain or shortness of breath, ④ one-sided leg swelling, ⑤ fever over 38°C, or ⑥ unusually heavy bleeding. These may indicate serious conditions such as thrombosis, so do not wait—contact a doctor immediately.
Other red flags include persistent nausea preventing fluid intake, severe headaches lasting more than two days, or worsening depression. For about two weeks after treatment, stay alert to any unusual symptoms. Never ignore your body’s signals—early consultation with a doctor is the safest approach.
Trying to Conceive and Fertility Treatment With a Planovar Period Reset

A Planovar period reset is closely related to pregnancy planning and fertility treatments. Let’s review the key points to efficiently move toward future conception.
- Cycle schedule for those aiming to conceive
- How it is used in IVF and timed intercourse treatments
- Precautions when combined with ovulation disorders or PCOS
Cycle Schedule When Aiming for Pregnancy
“After a period reset, when can I start trying to conceive? When will ovulation occur?” This is a crucial concern. After withdrawal bleeding ends, the next cycle begins the following day. Ovulation typically occurs on cycle days 12–16, making this the optimal window for conception. For example, if withdrawal bleeding lasts five days, ovulation is expected about two weeks after it ends.
To pinpoint ovulation, begin daily basal body temperature checks right after bleeding stops. Ovulation test kits are also very helpful. Depending on the severity of ovulatory dysfunction, doctors may prescribe ovulation induction agents (such as clomiphene). For women with irregular cycles, a Planovar reset can make ovulation timing easier to predict, providing a clear benefit for fertility planning.
Using Planovar in IVF and Timed Intercourse Treatments
“How does Planovar fit into fertility treatments?” In assisted reproductive technologies like IVF, Planovar is sometimes used to set a clear treatment cycle start date. For patients with irregular cycles, predicting the next menstruation is difficult, but Planovar ensures a planned reset, improving efficiency.
For example, in IVF, ovarian stimulation drugs are often started on day 3 of bleeding. With Planovar, this date can be fixed accurately. In timed intercourse treatments, the reset also makes ovulation more predictable, improving success in planning. However, since Planovar temporarily suppresses ovarian function, frequency and duration of use must follow the instructions of a fertility specialist. Overuse may affect ovarian function, so balance within the entire treatment plan is essential.
Precautions When Combined With Ovulation Disorders or PCOS
“What should I be careful about if I have ovulation disorders?” This is especially important. For women with ovulatory dysfunction or polycystic ovary syndrome (PCOS), continuous medical supervision is necessary. Even after a reset, natural ovulation may not occur, making planned use of ovulation inducers (like clomiphene or letrozole) important. For PCOS patients, insulin resistance often plays a role, so combining Planovar with insulin-sensitizing drugs (such as metformin), plus diet and exercise, can be more effective than Planovar alone.
Since ovulation tends to occur later than usual, regular ultrasound follicle monitoring is recommended in addition to basal body temperature checks. Because severity and causes differ for each woman, individualized treatment planning with your doctor is the fastest path toward successful conception.
Lifestyle Support: How to Balance Hormones Naturally

To maximize the benefits of Planovar and minimize side effects, lifestyle adjustments are important. By optimizing diet, sleep, and exercise, you can help your hormones stay balanced naturally.
- Nutrients and meal ideas to support a period reset
- Tips on sleep and stress management to reduce side effects
- Effective use of exercise, supplements, and Kampo (Japanese herbal medicine)
Nutrients and Meal Examples During a Period Reset
“What should I eat while taking Planovar? Can diet reduce side effects?” To balance hormones, focus on high-quality protein and antioxidants. Examples include fatty fish rich in omega-3s (such as mackerel or salmon), whole grains and legumes rich in B-vitamins, nuts and small fish for magnesium and calcium, and colorful vegetables packed with fiber and vitamins.
Sample menus include: salmon and avocado salad with flaxseed oil, steamed vegetables with multigrain rice, or yogurt with nuts and berries. For nausea relief, ginger soup, herbal teas, or lightly salted crackers can be helpful. On the other hand, caffeine, alcohol, processed foods, and sugary snacks may worsen side effects, so limit them during treatment. Also, aim for 1.5–2 liters of water daily to reduce swelling and support detoxification.
Reducing Side Effects Through Sleep and Stress Management
“How can I avoid side effects as much as possible?” Quality sleep and stress control are directly linked to reducing side effects. Sleep tips include going to bed and waking up at consistent times, avoiding blue light from phones or PCs 1–2 hours before bed, and keeping your bedroom cool (18–20°C), dark, and quiet.
For stress relief, try “5-minute breathing meditation,” stretching your shoulders and neck, or listening to your favorite music. If you feel emotionally unstable, practice mindfulness: notice the feeling (“I am anxious now”), then take three deep breaths. Talking with your partner or a trusted friend also helps maintain mental stability. If you struggle, don’t hesitate to consult your gynecologist for personalized advice.
Effective Use of Exercise, Supplements, and Kampo
“Besides medication, what else can help me stay balanced?” Complementary approaches include moderate exercise such as walking, yoga, or Pilates. These promote blood circulation and stabilize hormones. Yoga poses that improve pelvic blood flow (like the butterfly pose or child’s pose) can also reduce menstrual pain. Avoid intense workouts—aim for “slightly out of breath” intensity, about 20–30 minutes, 3–4 times per week.
With supplements, discuss with your doctor the use of iron, B-vitamins, magnesium, or omega-3 fatty acids, but avoid overdosing. In Kampo (traditional Japanese herbal medicine), Toki-shakuyaku-san (当帰芍薬散, for cold sensitivity) and Keishi-bukuryo-gan (桂枝茯苓丸, for swelling and cramps) are sometimes used. Always confirm compatibility with Planovar before combining. Personalized care—choosing the right mix of exercise, supplements, and herbal support—is the most effective path to better health.
Learn more about combining Planovar with other treatments ≫
Planovar Period Reset Q&A: Doctors Answer Common Questions

Here are the most frequently asked questions from patients about taking Planovar, along with medical explanations. Understanding the answers will help you feel more secure during treatment.
- Reasons and solutions when your period does not come or is delayed
- Sexual intercourse and contraception during treatment
- Safety and frequency of repeated use
Why Didn’t My Period Come? Reasons and Solutions
“I took Planovar but my period hasn’t come—should I be worried?” It’s not uncommon. If more than 5 days pass after the last dose without menstruation, possible causes include: ① individual hormonal response, ② strong stress or fatigue, ③ rapid weight changes, ④ thyroid dysfunction, ⑤ in rare cases, poor absorption of the medication.
First, if sexual activity occurred, use a pregnancy test kit to rule out pregnancy. If negative, stay hydrated, do light exercise, and make time to relax for about a week. If menstruation still doesn’t occur, consult a gynecologist for ultrasound or hormone tests. Some first-time users have weaker responses, so one attempt alone does not mean it is ineffective—future adjustments should be made together with your doctor.
Learn more about delayed menstruation after Planovar ≫
Sexual Intercourse and Contraception During Treatment
“Is sex safe while taking Planovar? Do I still need contraception?” Intercourse is medically possible during treatment, but contraception must be considered. Planovar does not provide reliable contraceptive protection like low-dose birth control pills.
Therefore, it is strongly recommended to use additional methods such as condoms during treatment and for about two weeks after finishing, until the next ovulation. Hormonal changes may also reduce vaginal lubrication, so water-based lubricants can help. Intercourse during withdrawal bleeding is best avoided, since it may increase infection risk or prolong bleeding. Communicate openly with your partner for safety and comfort. For couples trying to conceive, consult your doctor about timing after withdrawal bleeding.
Is It Safe to Use Planovar Repeatedly?
“Can I reset my period many times? How often is safe?” In general, Planovar is considered safe at a frequency of about once every 3–4 months. However, safety varies depending on age, health, and risk factors. People with high blood pressure, smokers, those over 35, or with a history of thrombosis require extra caution. Continuous or monthly use is not recommended.
For long-term cycle control, low-dose pills may be a better option. Ultimately, the key is to identify the root cause of irregular menstruation and treat it alongside lifestyle changes. Rather than temporary fixes, comprehensive management with your physician will bring the best results.
Consultation Guide: Online Appointments and Choosing a Gynecology Clinic

To receive a prescription for Planovar, choosing the right gynecology clinic is essential. Here are practical tips on selecting a medical facility and using online consultations effectively.
- Pros and cons of online consultations
- Five key points for choosing a clinic
- Latest costs and insurance coverage
Pros and Cons of Online Consultations
“I don’t have time to visit a clinic—can I get a prescription online? What are the benefits and risks?” The greatest advantages of online consultations are time savings and easier scheduling. This is especially useful for those who cannot visit a hospital during working hours or feel uneasy about in-person gynecology visits. Benefits include no waiting rooms, reduced infection risk, and home delivery of medication.
However, the limitations are that initial exams cannot include physical checks such as ultrasounds or pelvic exams, so in some cases you may still need to visit a clinic. Other considerations include unstable internet connections, more difficult patient–doctor communication compared to in-person visits, and higher out-of-pocket costs if not covered by insurance. For simple cycle adjustments with Planovar, online consultations are often sufficient, but for complex cases such as ovulation disorders, an in-person visit is recommended.
Five Key Points for Choosing a Clinic
“What should I look for in a gynecology clinic?” First and foremost, check the clinic’s specialty. Look for gynecologists experienced in irregular menstruation or ovulation disorders, and confirm qualifications such as reproductive medicine certification. Past achievements in infertility or hormone treatments are also good indicators.
Second, assess convenience: Does the clinic allow online booking? What is the expected wait time? What initial tests are performed? Choose a system that fits your lifestyle.
Third, consider the doctor’s approach and communication: Do they explain thoroughly? Do they respect patient wishes and lifestyle? Are questions answered clearly? Patient reviews and your first impression are valuable indicators.
Fourth, check accessibility and office hours. Evening or weekend appointments can be crucial for working women.
Fifth, evaluate facilities and privacy. High-quality ultrasound equipment and private consultation rooms are reassuring. Considering all these factors helps you find a trusted “primary gynecologist” for long-term health management.
Latest Costs and Insurance Coverage
“How much does a Planovar prescription cost? Can I use insurance?” Costs vary depending on whether the treatment qualifies for insurance coverage. For medical purposes such as irregular menstruation or ovulation disorders, insurance usually applies. Typical fees include: initial consultation (about ¥1,000–2,000), follow-up visits (¥500–1,000), and medication (about ¥1,000–1,500 for 10 days). Total: ¥3,000–4,500.
For non-medical reasons, such as adjusting menstruation for a wedding or travel, the cost is usually out-of-pocket. Clinics may charge ¥5,000–8,000, including consultation and medication. For online consultations, first visits often cost ¥5,000–7,000, and follow-ups ¥3,000–5,000. Additional tests, such as ultrasound (¥3,000–5,000) or hormone tests (¥5,000–10,000), may be required.
Since fees vary, check the clinic’s website or call in advance. At your first visit, confirm whether insurance applies and what tests are needed to avoid unexpected costs.
Conclusion

With the right knowledge and preparation, a Planovar period reset can be a reliable way to adjust your cycle for important events. This article has explained the mechanism of Planovar, practical scheduling, side effect management, how it relates to fertility, and lifestyle habits that support hormonal balance.
Key takeaways include:
- Menstruation usually begins 2–4 days after the last dose.
- To reduce side effects, take the pill at bedtime and stay well-hydrated.
- For important events, schedule adjustments with at least 3 weeks’ margin.
- After a reset, ovulation typically occurs about two weeks into the new cycle.
Every woman’s body and lifestyle are different. If you feel uncertain, consult your gynecologist—especially for first-time use or when planning around significant life events. At Personal Care Clinic, we offer counseling to design a personalized Planovar reset plan tailored to your goals.
Related Articles