“Morning nausea makes me want to quit Planovar right now… but is it safe to stop on my own?”
Among people taking Planovar (プラノバール, Puranobāru) for irregular periods or menstrual pain, quite a few struggle with the side effect of nausea. When daily nausea keeps you from focusing at work or enjoying meals with friends, it’s natural to feel “I want to stop.”
This article answers common questions many people have while taking Planovar:
- Why does Planovar cause nausea, and how long does it last?
- Can I ease the nausea without stopping the medication?
- How should I talk with a doctor to stop safely?
We’ll cover the causes and remedies for Planovar-related nausea, safe discontinuation steps, and possible alternatives, using clinician-reviewed information. At Personal Care Clinic, we also offer individualized consultations to match your symptoms and lifestyle. Let’s explore ways to get relief from nausea first.

At Personal Care Clinic, the morning-after pill can be delivered in as little as 37 minutes.
The prescription process takes just 5 minutes, and if you apply before 10:30 AM, same-day pickup is available (depending on your area).
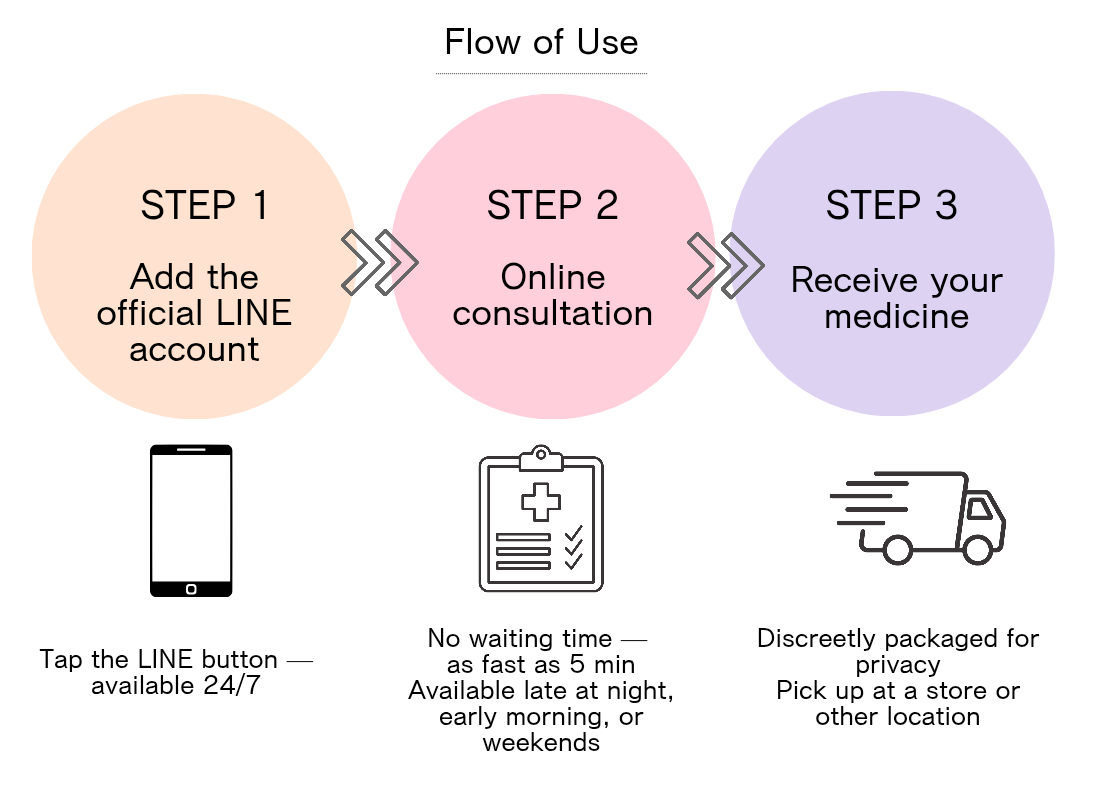
If you want to receive the morning-after pill discreetly, tap the button below to apply now.
Planovar Nausea—Want to Stop? A Complete Guide to Causes and Relief Steps

Many people suffering from Planovar-related nausea feel “I want to stop.” Before you do, understanding the cause and countermeasures may reduce symptoms enough to continue treatment. First, learn the basics of Planovar and the mechanism of nausea.
- What is Planovar? Basics of a medium-dose pill and how side effects arise
- Three mechanisms behind nausea and their risk levels
- What to watch for at different moments when you “want to stop”
What Is Planovar? Basics of a Medium-Dose Pill and How Side Effects Arise
“So what exactly is Planovar?” Let’s start there!
Planovar is a medium-dose pill containing two female hormones—estrogen and progestin. Because it has higher hormone amounts than low-dose pills, it is effective for conditions like dysmenorrhea and endometriosis.
However, the higher hormone dose is also linked to side effects. Once in the body, these hormones can act on the brain’s vomiting center, causing nausea—especially early in treatment. This is similar to the mechanism behind morning sickness.
Side-effect intensity varies from person to person, and often eases as your body adapts. If symptoms don’t improve after three months, use that as a cue to consult your clinician.
Three Mechanisms Behind Nausea and the Risk Levels
“Why is my nausea worse than others’?” Understanding the reasons makes planning countermeasures easier!
Nausea with Planovar generally arises through three mechanisms:
1. Hormonal fluctuation: Estrogen directly stimulates the brain’s vomiting center. Weeks 1–3 after starting are often the toughest.
2. GI effects: Hormones can slow stomach motility, delaying digestion—often worse when taken on an empty stomach.
3. Individual sensitivity: People sensitive to hormonal shifts or prone to motion sickness may feel more nausea.
As for risk levels, about 15–20% of users experience some nausea, while severe, daily-life-limiting symptoms occur in roughly 5%.
More on medium-dose pill side effects ≫
What to Watch for When You “Want to Stop,” by Timing
“I want to quit now!” We get it—but the right response depends on timing.
If it’s within the first month: early nausea is often temporary. If you can, continue up to three months; many people adapt by then.
At three months or more: if nausea persists even after adaptation, ask your doctor about dose adjustments or switching. Stopping on your own can abruptly disrupt your hormone balance.
On long-term use (≥1 year): stopping suddenly may trigger irregular periods or a return of prior symptoms. Reduce gradually under medical guidance.
Five First-Aid Tips Before You Stop Planovar for Nausea

Before discontinuing, try ways to lessen nausea. Many find they can continue therapy after simple changes. Here are practical, quick-start strategies.
- Relief by adjusting dose timing, meals, and hydration
- Are OTC anti-nausea options okay alongside Planovar?
- How to use vitamin B6, ginger, and Kampo remedies
Relief With Timing, Meals, and Hydration
“Can small tweaks really cut nausea?” Yes—routine adjustments can help a lot.
The easiest, often effective tactic is to change how you take Planovar:
First, take it at bedtime so the worst nausea passes while you sleep. Many feel better on waking.
Avoid taking it on an empty stomach; take it with a light meal. Carbs like crackers or bread can buffer the stomach.
Hydration matters: rather than a large gulp at once, sip water slowly after the dose to reduce stomach load.
In the morning, rise slowly rather than jumping out of bed. These steps help many people feel meaningful relief.
Are OTC Anti-Nausea Options Okay? Pharmacist-Recommended Choices
“Can I use over-the-counter meds safely?” Here’s what pharmacists often suggest.
Some anti-nausea medicines can be combined with Planovar, but not all are safe—use caution.
Pharmacists often recommend metoclopramide, which promotes gastric emptying. Note: this is a prescription drug.
Over-the-counter motion-sickness products (e.g., dimenhydrinate brands) may help temporarily, but can cause drowsiness—use care before work or driving.
Whatever you choose, always consult your clinician first. Self-directed combinations can cause unexpected adverse effects.
Vitamin B6, Ginger, and Kampo—How to Use Supplements
“Is there a natural way to calm nausea?” Yes—some options are worth trying.
For hormone-related nausea, vitamin B6 can help; studies on morning sickness support it. Consider 25–50 mg/day.
Ginger is a classic anti-nausea aid—tea, candies, or supplements. If mornings are tough, try ginger tea right after waking.
In Kampo, Hangeshashinto (半夏瀉心湯, Hangeshashintō) is used for GI upset and nausea. It requires a prescription and a fit assessment by a physician.
Personal Care Clinic can advise on the best-fit supplements or Kampo for your body type, while continuing hormone therapy but easing nausea.
Safe Steps to Stop Planovar When Nausea Makes You Want to Quit

If nausea does not improve despite multiple strategies, you may decide to stop Planovar. Avoid self-discontinuation; here’s how to stop safely under medical guidance.
- Risks of stopping on your own and doctor-recommended steps
- Checklist of symptoms to report at your visit
- Body changes after stopping and how to manage them
Risks of Self-Stopping and Doctor-Recommended Steps
“I can’t stand it—want to quit now!” We understand—but please pause.
Stopping Planovar abruptly on your own carries several risks: sudden hormone shifts can trigger breakthrough bleeding or a return of severe cramps. Underlying conditions (e.g., endometriosis, irregular cycles) may also flare.
Doctors generally advise these safer steps:
1. Finish your current pack; don’t stop mid-pack.
2. Do not start the next pack; book a medical visit.
3. At the visit, describe your symptoms and circumstances in detail.
4. Based on evaluation, you may taper or switch to alternatives.
For long-term users, gradual tapering is often preferred to avoid abrupt hormonal shifts.
Checklist of Symptoms to Report at Your Visit
“What should I tell my doctor?” Use this checklist.
At your appointment, communicate specifics using this symptom checklist:
□ Nausea frequency (daily, several times per week, etc.)
□ Timing (morning, right after dosing, all day, etc.)
□ Intensity (impact on daily life)
□ Any actual vomiting
□ What you’ve tried so far and effects
□ Other side effects (headache, dizziness, swelling, etc.)
□ Duration of use and recent life changes
□ Whether you plan pregnancy soon
Also share any gynecologic symptoms (cramps, spotting). That helps risk assessment and choosing alternatives. Bring notes or a symptom diary for accuracy.
Body Changes After Stopping and How to Handle Them
“What happens after I stop—and how should I prepare?” Planning ahead makes it smoother.
Post-Planovar changes vary, but knowing common patterns helps.
Consider the first 1–3 months as an adjustment while your hormones stabilize. Possible changes include:
1. Cycle changes: periods may be irregular or absent. If there’s no period for >3 months, consult your doctor.
2. Return of cramps: prior pain can come back; prepare heat therapy and analgesics.
3. Acne flare: hormonal shifts can trigger skin trouble—adjust skincare.
4. Mood shifts: irritability or low mood—prioritize sleep and stress management.
Balanced meals, moderate exercise, and good sleep help. Plan follow-ups for about three months after stopping.
If You Want to Quit Planovar—Compare Alternative Pills and Treatments

Even if Planovar-related nausea is tough, you may still need treatment for the original issues (pain or irregularity). Here we compare alternatives so you can find a good fit.
- Comparison table of low-dose pills and mini-pills
- Non-hormonal cycle management (IUD, analgesics)
- Real-world differences in cost, access, and visit frequency
Low-Dose Pills vs. Mini-Pills: Features and Side-Effect Comparison
“Will switching pills reduce nausea?” Know the differences to choose well.
Alternatives to Planovar (a medium-dose pill) include low-dose combined pills and progestin-only mini-pills. Compare their features and side effects:
[Low-dose combined pills]
・Feature: therapeutic effect with less hormone than Planovar
・Nausea risk: about half that of medium-dose pills
More on low-dose pill side effects ≫
・Benefits: reduces cramps and menstrual flow
・Representative brands: Marvelon, Triquilar
・Best for: those seeking contraception and cycle control
[Mini-pills (progestin-only)]
・Feature: contains no estrogen; progestin only
・Nausea risk: lowest (~≤5%)
・Benefits: effective contraception; flow-reduction effect slightly weaker than low-dose combined pills
・Representative brand: Cerazette
・Best for: estrogen-sensitive people, those with strong nausea, or those who are breastfeeding
If nausea is the main issue, pills with less—or no—estrogen, such as mini-pills, are often recommended. Note the trade-off of more spotting.
Non-Hormonal Options (IUD, Analgesics)
“Are there non-hormonal choices?” Yes—consider these.
[Hormone-releasing IUD]
・Feature: placed in the uterus; releases hormone locally
・Pros: fewer systemic side effects; long-acting (3–5 years)
・Cons: insertion pain; initial spotting
・Best for: those wanting a long-term solution or who struggle with daily pills
[Analgesic therapy]
・Feature: planned NSAID use
・Pros: take only when needed; no hormonal impact
・Cons: symptomatic, not causal; GI-upset risk
・Best for: mainly pain without other cycle issues
[Kampo medicine]
・Feature: aims at whole-body balance
・Pros: relatively fewer side effects
・Cons: benefits may take time
・Best for: those who prefer natural, long-term body-balance approaches
Suitability varies by symptoms, constitution, and lifestyle. Decide with a specialist.
Real-World Differences: Cost, Access, and Visit Frequency
“Will switching raise costs or clinic visits?” Let’s compare with practical numbers.
When choosing a therapy, consider cost and convenience as well as effect:
[Approximate 3-month costs]
・Planovar: ¥3,000–4,500 (when covered by insurance)
・Low-dose pills: ~¥3,000–9,000 (often not covered for contraception)
・Mini-pills: ~¥4,500–6,000 (not covered)
・Hormone-releasing IUD: ~¥30,000–50,000 initial (then 3–5 years of effect)
・Analgesics: ~¥1,500–3,000
・Kampo: ~¥3,000–7,000 (when covered)
[Access and visit frequency]
・Planovar: follow-ups every 1–3 months
・Low-dose pills: follow-ups every 1–3 months; telemedicine may be available
・Mini-pills: follow-ups every 1–3 months; telemedicine may be available
・Hormone-releasing IUD: insertion plus periodic checks (every 6–12 months)
・Analgesics: as needed; some OTC options
・Kampo: typically every 1–2 months
Insurance coverage (using Japan’s system and a health insurance card) also matters. Planovar is often covered for dysmenorrhea or endometriosis treatment; low-dose pills for contraception are usually not. Fees vary by clinic—check in advance.
Lifestyle Improvements to Tackle Planovar-Related Nausea at the Root

Beyond dose tweaks, daily habits help. Nutrition, sleep, and exercise can steady hormones and reduce side effects.
- Balanced meals and low-GI choices to smooth hormone swings
- Why sleep and stress care reduce side effects
- Light exercise and breathing to calm nausea
Balanced Meals and Low-GI Foods
“Can food choices change nausea?” Yes—they can make a big difference.
Review diet to ease Planovar-related nausea. Big swings in blood sugar may worsen symptoms.
Low-GI staples help stabilize hormones:
・Whole grains (brown rice, whole-wheat bread)
・Legumes (natto, tofu, chickpeas)
・Non-starchy veg (broccoli, spinach)
・Quality protein (chicken, fish, eggs)
Eat small amounts more often to reduce stomach load. In the morning, avoid an empty stomach—try some crackers or easy-to-digest biscuits right after waking.
Foods to limit:
・Greasy foods (slow gastric emptying)
・Very spicy dishes
・Caffeine (stimulates acid)
・Alcohol (irritates mucosa)
Keep a food diary to see what helps or worsens symptoms.
Why Sleep and Stress Care Matter
“Can better sleep really help?” Yes—sleep quality influences side effects.
Good sleep helps regulate hormones and supports detox functions. Aim for 7–8 hours; sleep between ~10 p.m. and 2 a.m. is especially helpful for hormonal balance.
Excess cortisol from stress can slow digestion and worsen nausea. Stress care isn’t just mood—it affects the body directly.
Tips:
・Avoid blue light before bed
・Keep your bedroom ~18–20 °C
・Go to bed at a consistent time
・Try calming herbal teas (chamomile, lavender)
・Practice 10 minutes of meditation or deep breathing
If dosing at bedtime, lie down and relax soon after to minimize night nausea.
Light Exercise and Breathing to Calm Nausea
“Won’t movement worsen nausea?” The right activity can actually help.
Appropriate exercise can reduce symptoms; light to moderate aerobic activity balances stress hormones and supports digestion.
Recommended:
・Walking (15–20 minutes after meals)
・Gentle yoga (digestive poses)
・Stretching (full-body in the morning)
・Light body-weight training
Breathing you can do anytime:
[4-7-8 breathing]
1. Inhale through the nose for 4 seconds
2. Hold for 7 seconds
3. Exhale through the mouth for 8 seconds
4. Repeat four times
This activates the parasympathetic system and can ease nausea. Try it before getting out of bed.
Building these habits can improve not only side effects but overall well-being. Start small and make it routine.
Planovar Nausea & Stopping—Top 10 FAQs

Here are evidence-based answers to common questions about Planovar-related nausea and stopping the medication.
- How long does nausea last? Typical timelines and variation
- Is it okay if I’m trying to conceive? How to re-plan treatment
- Next steps if anti-nausea meds don’t work
How Long Does Nausea Last?
“Will this nausea last forever?” No—most improve over time.
Here’s what clinical trends and experience suggest:
[Typical course]
・Weeks 1–2: most people peak here, then improve
・1–3 months: about 70% improve as the body adapts
・>3 months: about 15–20% still have nausea
Factors affecting variation:
・Baseline hormone sensitivity
・GI condition
・Stress level
・Dosing method (with/without food; morning/night)
Note how timing and meals can change nausea even on the same drug. Many improve by switching dosing to night.
If there’s no improvement after three months, consult your doctor about alternatives—adaptation isn’t guaranteed for everyone.
Trying to Conceive? How to Re-Plan
“I want to start TTC—what should I do with Planovar?” Plan a timed switch.
Key steps for a pregnancy plan:
[Stopping plan for TTC]
1. Pre-consultation (3–6 months ahead):
Tell your clinician when you hope to stop. Learn basal-body-temperature tracking and ovulation checks.
2. Start folic acid:
Begin 400–800 µg/day three months before stopping to lower neural-tube-defect risk.
3. Gradual discontinuation:
Your clinician may taper to avoid abrupt shifts.
4. Observe cycles:
Natural cycles may take 1–3 months to return. Track basal temperature.
5. Fertility support:
Consider ovulation-induction or other supports if needed.
Give your body time to regain rhythm before trying to conceive.
If Anti-Nausea Measures Don’t Work
“I tried everything and nothing helps.” There are still options.
Consider these next steps:
1. Reassess hormone dose with a specialist:
Discuss lower-estrogen pills or alternate-day adjustments.
2. Prescription anti-nausea therapy:
Stronger options like metoclopramide may help when OTC meds fail.
3. Switch to alternatives:
Mini-pills or low-dose combined pills with less estrogen can help if estrogen is the main trigger.
4. Non-hormonal approaches:
Kampo or non-hormonal analgesics if hormonal therapies don’t suit you.
5. Second opinion:
Consult another specialist—preferably with strong women’s-hormone expertise.
Don’t resign yourself—modern care offers many options.
Summary

Nausea from Planovar is common, but with the right strategies and clinical support, it can improve or be resolved. We covered causes, practical remedies, safe discontinuation, and alternative options.
Key points:
1. Understand causes and adjust timing and meals—many feel better.
2. If there’s no improvement after three months, it’s time to consult about alternatives.
3. Don’t stop on your own—make changes under medical guidance.
4. Consider low-dose pills or mini-pills for fewer side effects.
5. Lifestyle upgrades—diet, sleep, exercise—also help.
Resources you may find especially useful:
- Relief with timing/meals/hydration
- Vitamin B6, ginger, and Kampo strategies
- Comparison of low-dose pills and mini-pills
Treating menstrual pain or irregular cycles matters—but your daily life matters too. If nausea is disrupting your routine, don’t carry the burden alone—consult a specialist at Personal Care Clinic. Together we can find a treatment that fits your body and lifestyle. Today can be your first step back to comfort.
Related Articles